The stress test (or ergometry) is a test in which the electrical activity of the heart is recorded while you walk or run on a treadmill, or pedal a stationary bicycle. It is used to assess how your heart responds to exercise and whether signs of ischemia (lack of irrigation), arrhythmias or other changes that are not seen at rest.
In this guide you will see when indicated, how you should get ready, What are the real risks and what kind of information does it provide for your diagnosis and treatment?.
Brief warning: This text is informative and does not replace your medical evaluation. The indication and protocol of your stress test must be discussed individually with your cardiologist.
What is a stress test and what is it for?
During the stress test:
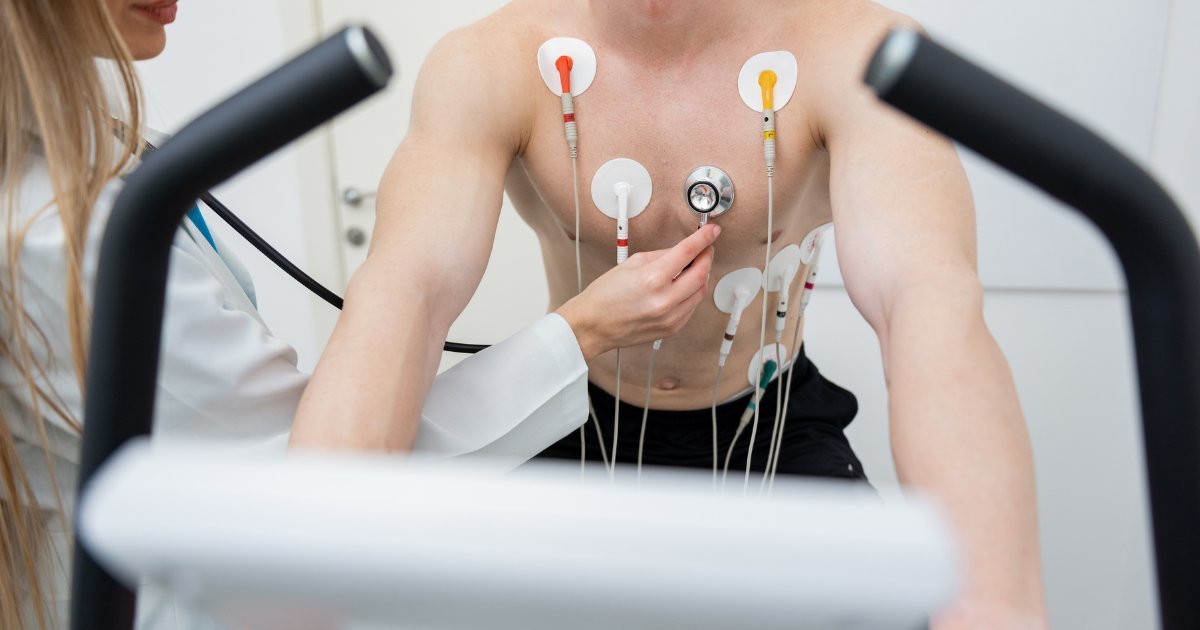
- You are connected to a continuous electrocardiogram.
- You walk or run on a treadmill that gradually increases in speed and incline (or pedal a bicycle).
- They measure your heart rate, blood pressure and symptoms at each stage.
The test helps answer questions such as:
- Does chest pain or shortness of breath occur with exercise?
- Does the ECG show signs of ischemia by demanding the heart?
- Are they triggered arrhythmias with the effort?
- What is your functional capacity approximate (how many METs do you reach)?
When well indicated and supervised, it is a very useful tool for:
- Study chest pain suspicious of cardiac origin.
- Rate coronary risk in certain patients.
- Evaluate whether it is safe to start or intensify an exercise program.
- Assist in the design of a plan in the context of Cardiac rehabilitation.
More technical details can be found on the studio's website: Cardiac stress test (Ergometry).
In which cases is a stress test usually indicated?
The idea is not to “make it routine” to everyone, but when it answers a specific question. Some typical scenarios:
- Chest pain or discomfort on exertion
- Oppressive discomfort, burning or pressure in the chest when climbing stairs or walking fast.
- The aim is to see if the effort causes changes in the ECG that suggest obstructions in the coronary arteries.
- Dyspnea (shortness of breath) with moderate activity
- When it is not clear whether the cause is cardiological, pulmonary, physical deconditioning or other.
- The heart's response to exercise provides important clues.
- Evaluation before starting intense exercise or sport
- Especially in patients over a certain age or with risk factors.
- It can be integrated into a Pre-sports Cardiovascular Evaluation.
- Follow-up in known coronary artery disease
- To assess response to treatment, functional capacity and risk.
- Adjustment of the Cardiac rehabilitation
- Helps to define safe intensity zones for exercise.
In many people, the stress test is part of an overall cardiological check-up not from a “generic package”.
How to prepare for a stress test
Your cardiologist will give you specific indications, but in general:
- Clothing and footwear
- Wear comfortable and light clothing.
- Wear tennis shoes or stable sports shoes.
- Pre-feeding
- Avoid very abundant meals in the 2-3 hours before.
- Do not arrive with prolonged fasting (so as not to get dizzy).
- Medications
- Some drugs, such as certain beta-blockers, can modify the heart's response to exercise.
- NEVER discontinue medications on your own: your cardiologist will tell you whether you should take the usual dose or make any adjustments.
- Caffeine, tobacco and alcohol
- It is usually recommended to avoid caffeine and tobacco a few hours beforehand.
- Do not show up with a hangover or under the influence of alcohol.
- Rest
- Get a reasonably good night's sleep the night before, as far as possible.
If you have specific doubts (e.g., you are under treatment with multiple drugs or have a pacemaker), it is ideal to clarify them in the previous consultation.
How the study is performed, step by step
A typical stress test scheme:
- Initial assessment at rest
- Brief review of symptoms, history and current medications.
- A Electrocardiogram (ECG) basal and blood pressure is taken.
- Placement of electrodes and band
- Stickers are placed on the chest connected to the monitor.
- You are placed on the band or bike and the protocol is explained.
- Stages of progressive exercise
- Speed and inclination increase in stages (e.g., every 3 minutes).
- ECG, heart rate, pressure and symptoms are recorded at each stage.
- The test is stopped if:
- You reach your target heart rate.
- You present important symptoms.
- The ECG shows changes that warrant stopping exertion.
- Recovery phase
- Monitoring continues as the rhythm and pressure return to baseline.
- This part also provides valuable information (e.g., slow heart rate recovery).
The total duration in the laboratory is usually 30 to 60 minutes, although the exercise time is shorter.
Real risks of the stress test
It is normal to feel some trepidation at the thought of “straining” your heart in a study, especially if you already have symptoms. Key points about risks:
- In the vast majority of patients, the test runs without complications.
- There is a very low risk of events such as significant arrhythmias, severe angina or, in very rare cases, infarction.
- Precisely because of this:
- The study is conducted in a controlled environment.
- Trained personnel and emergency equipment are available.
- The test is stopped as soon as alarm data appears.
Before indicating it, your cardiologist evaluates if the expected benefit (diagnostic information, treatment guide) far outweighs the risk, and whether this risk is acceptable in your particular case.
What kind of results can you expect
A stress test report may include data such as:
- Functional capacity (METs achieved).
- Whether or not typical chest pain during exercise.
- Presence of changes in the ST or other ECG alterations suggestive of ischemia.
- Appearance of arrhythmias (supraventricular or ventricular) triggered by exertion.
- Response from the blood pressure (normal, exaggerated, hypotensive).
- Time of heart rate recovery.
With this, your cardiologist can:
- Estimate your coronary risk with greater precision.
- Decide whether you require additional studies (e.g., imaging tests) or treatment adjustment.
- Define safe exercise areas and integrate, if appropriate, into a training program. Cardiac rehabilitation.
When is NOT the right time for a stress test?
There are situations in which a stress test is contraindicated or should be postponed:
- Typical chest pain at rest or suspected acute myocardial infarction in progress.
- Unstable arrhythmias, decompensation of heart failure or hypertensive crisis.
- Some severe untreated valvular conditions.
In these scenarios, the priority is the urgent care or stabilization, not the programmed effort.
How do you know if you need it?
You may be a candidate for a stress test if:
- You have chest discomfort or shortness of breath that appears with exertion.
- You plan to start or increase an exercise program and have risk factors (age, hypertension, diabetes, high cholesterol, smoking, family history).
- You have already been diagnosed with coronary artery disease and your cardiologist wants to assess functional capacity and response to treatment.
If you recognize yourself in any of these points, you can comment on them during your cardiological check-up or request more information directly through the contact.
References
- 2012 ACCF/AHA Guideline for the Diagnosis and Management of Patients With Stable Ischemic Heart Disease (Circulation):
https://www.ahajournals.org/doi/10.1161/CIR.0b013e318277d6a0 - Gibbons et al. ACC/AHA 2002 Guideline Update for Exercise Testing (Circulation):
https://www.ahajournals.org/doi/10.1161/01.CIR.0000041700.29784.3C - Arena et al. Assessment of functional capacity in clinical cardiology (Circulation):
https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.110.949131