By Dr. Karla Moraima Castolo - Clinical Cardiologist
Know your credentials
The heart failure does not mean to stop moving. On the contrary, the supervised exercise is one of the pillars of modern treatment: it improves functional capacity, quality of life and can reduce hospitalizations. But it must be initiated gradually and in a controlled manner, following specific clinical parameters and without improvising routines.
For a plan adapted to your condition and safety, schedule your assessment.
TL;DR
- The exercise is safe and beneficial if it is individualized and monitored.
- Starts with short walks, The time and frequency of the treatment will increase progressively.
- Avoid maximum stress or extreme heat/cold environments.
- Learn to identify warning signsDyspnea: severe dyspnea, dizziness, sustained palpitations or disproportionate fatigue.
- The cardiac rehabilitation is the safest environment to start or resume activity.
Why exercise helps in heart failure
Regular physical training improves the efficiency of the heart and peripheral circulation. It increases exertional capacity (VO₂ peak), reduces symptoms such as fatigue and improves mood. Guidelines recommend incorporating it as part of standard treatment along with medication, fluid management and patient education.
The key is the precise dosingThe type, intensity, frequency and duration should be defined according to your functional class (NYHA), ejection fraction and clinical stability.
Before you start
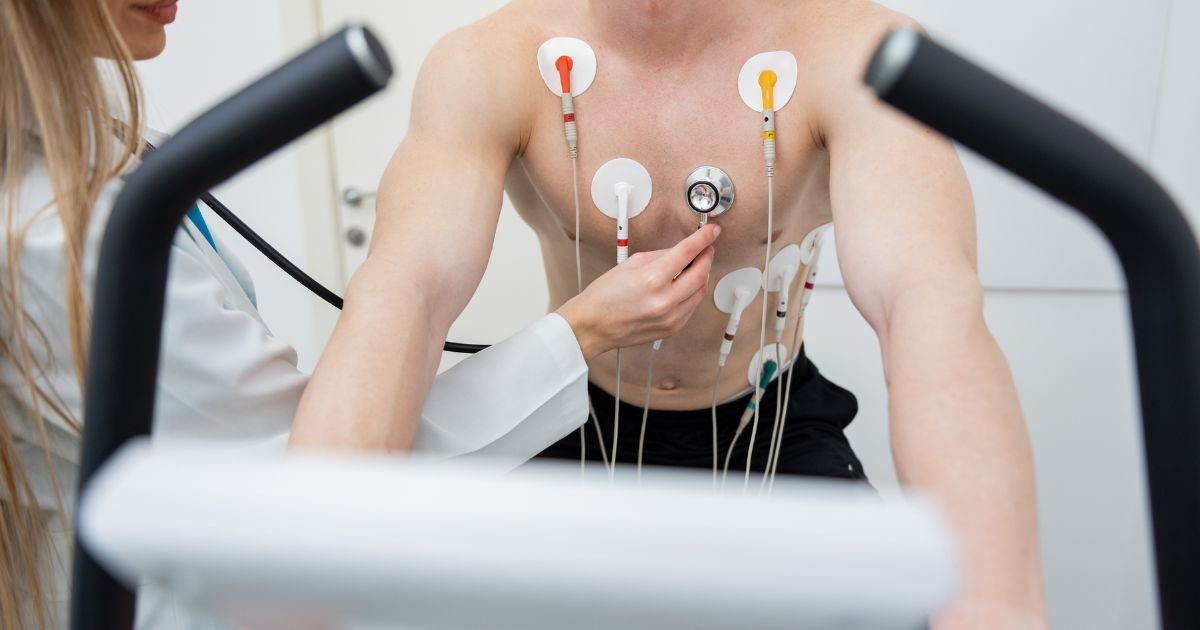
- Complete medical evaluationincludes physical examination, electrocardiogram and, in some cases, echocardiogram or symptom-limited stress test.
- Clinical stabilityno recent decompensation, no fluid retention or recent changes in medication.
- Initial educationKnow your warning signs and learn how to monitor your response.
- Suitable environmentideally within a program of supervised cardiac rehabilitation.
How to structure your program
Initial phase (weeks 1-3)
- Gentle walks of 10-15 minutes, 3-5 days/week.
- Intensity: you must be able to keep conversation short (perceived exertion 9-11/20 on Borg scale).
- Immediate rest in case of fatigue or dyspnea greater than usual.
Progression phase (weeks 4-8)
- Increases the time to 20-30 minutes per session.
- If you tolerate well, add low weight force (2×/week, large muscle groups, 10-15 repetitions).
- Avoid prolonged horizontal exercises if there is respiratory difficulty.
Maintenance phase (from week 9)
- 30-45 minutes, 4-5 times per week, combining walking, exercise bike or aquatic exercises.
- Moderate intensity: mild dyspnea and rapid recovery (<2 min).
- Periodically reevaluate your functional capacity and medication adjustments.
Alarm signals
Stop the activity and seek guidance if you present:
- Chest pain or tightness that does not subside.
- Severe or worsening dyspnea with respect to previous days.
- Dizziness, syncope or extreme fatigue.
- Sustained palpitations or unexpected tachycardia.
- Sudden weight gain (>2 kg in a few days) or marked swelling of legs or abdomen.
Practical recommendations
- Heats and cools 5-10 minutes before and after each session.
- Avoid extreme temperatures and exercise immediately after eating.
- Weigh and record your symptoms each day; report changes to the treating team.
- Wear light clothing and comfortable shoes.
- Do not discontinue medication without medical indication.
- Combine with self-care: adherence, low sodium diet and stress control.
Frequently Asked Questions
Can I exercise if I have a “weak heart”?
Yes, if you are stable and under medical supervision. Cardiac rehab adjusts intensity and frequency safely.
Does exercise replace medication?
No. It is a supplement that enhances its benefits and improves your functional capacity.
What type of exercise is best?
Walking, stationary cycling and light strength training are the safest. Avoid intense isometric or competitive exercises.
What happens if I get fatigued quickly?
Decrease the intensity, split the time and prioritize constancy. Improvement is progressive.
Can I train at home?
Yes, with initial instruction from your cardiologist or rehabilitation physiotherapist, monitoring symptoms and heart rate.
To get started in a safe and personalized way, schedule your assessment.
References
- CENETEC/SSA. (2022). Primary, secondary prevention and cardiac rehabilitation of cardiovascular disease (SS-152-22).
- Yancy, C. W., et al. (2017). 2017 ACC/AHA/HFSA Guideline for the Management of Heart Failure. Circulation.
- Piepoli, M. F., et al. (2016). Exercise training in heart failure: recommendations of the ESC Heart Failure Association. European Journal of Heart Failure.
- Taylor, R. S., et al. (2019). Exercise-based rehabilitation for heart failure: Cochrane Review. Cochrane Database of Systematic Reviews.
- World Health Organization (2020). Physical activity and cardiovascular health.